Intentional Replantation as the Treatment of Left Mandibular Second Premolar Refractory Periapical Periodontitis: A Case Report
Abstract
Introduction
This report aims to assess the feasibility of intentional replantation combined with concentrated growth factor(CGF) membrane treatment for refractory apical periodontitis of the left mandibular second premolar (35), with a 13-month follow-up period.
Case Report
A 24-year-old female patient underwent root canal treatment for pulpitis of the left mandibular second premolar 3 years ago, and her gum repeatedly swelled and drained pus after the treatment. CBCT revealed that the apical area of 35 was adjacent to mental foramina, and the cyst range was large. There could be issues of poor visual field, trauma, difficulty in apical preparation and backfilling after the apical resection. The left mandibular second premolar (35) was extracted, and the inflammatory tissues in the apical and alveolar fossa were removed, followed by the removal of apical irritants. The extracted premolar was then implanted into the alveolar fossa and fixed.
Results and Prognosis
After a duration of 13 months, the left mandibular second premolar 35 exhibited no clinical symptoms and was able to perform normal masticatory function. There was an absence of gum swelling, pain or mobility; cone beam computed tomography imaging revealed bone regeneration below the root apex with the absence of new lesions, root resorption, or adhesion to the alveolar bone. The periodontal ligament demonstrated healing between the root and alveolar bone, effectively controlling infection, preserving infected teeth and facilitating the formation of new attachments around them.
Discussion
Intentional tooth replantation has some advantages, like short operation time, less cost, less bone injury, and less limitations in terms of anatomy and location. However, clinicians should consider whether intentional replantation could be performed before dental implantation for the affected teeth with intractable periapical lesions. Nonetheless, its efficacy needs further evaluations through long-term clinical follow-ups.
1. INTRODUCTION
Following traumatic tooth injury and avulsion, replantation, which refers to reinserting a tooth into its original socket after treatment for extraction and removal, should be promptly performed. Replantation is widely recognized as an essential treatment method because of factors including the duration of extra-alveolar time, postextraction preservation environment, and replantation technique [1]. Dr. Grossman, in 1966, defined tooth replantation as “the deliberate extraction and immediate reinsertion of a tooth” aimed at sealing the root canal from an apical direction upon removal [2].
Intentional replantation was proposed by Grossman in 1982 [3]. It refers to the complete extraction of teeth that are otherwise difficult to cure by conventional methods. After a series of in vitro diagnoses, examinations, and treatments, it is implanted back into the original alveolar socket. The method preserves affected teeth. Intentional replantation is employed in refractory periapical periodontitis with persistent symptoms linked to the root canal, apical surgery, apical surgery with anatomic constraints, longitudinal root cleft or developmental malformation, lateral root canal perforation, instrument separation, and traumatic teeth. It is considered the last treatment resort to preserve affected teeth, control the infection, and restore chewing function [4]. The successful intentional replantation avoids the affected tooth removal as the conventional treatments are harder to implement or to completely remove the infected materials. This chronic periapical periodontitis case of the left second premolar fails in terms of root canal treatment, and apical surgery can also not be performed. Microscopic root canal therapy, intentional replantation, and nano-bioactive materials are employed for infection control, affected tooth preservation, and formation of new peridental attachments. This report aims to assess the feasibility of intentional replantation combined with CGF membrane treatment for refractory apical periodontitis of the left mandibular second premolar (35), with a 13-month follow-up period.
2. CASE REPORT
2.1. General Data
A 24-year-old female patient underwent root canal treatment in a hospital 3 years ago because of the “chronic pulpitis” of the left mandibular second premolar. The gum repeatedly swelled and drained pus after the treatment. The patient arrived at our department on March 25, 2022.
2.2. Clinical Examination
Oral hygiene was good. Thirty-five occlusal surface resin filling body was intact. There was knock pain (+-)but no loosening and gingival discomfort (Fig. 1). X-ray depicted that 35 canals had been filled, and the circular low-density shadows were visible in the apical area. The cone beam computed tomography (CBCT) exhibited suspicious images of instrument separation in the root apex of 35. The low-density images were found for the root apex area with clear boundaries in the proximity of the mandibular neural tube.
2.3. Diagnosis
Refractory periapical inflammation of the left mandibular second premolar 35.
The medical records and imaging data of root canal treatment for the left mandibular second premolar 35 were consulted. Considering that the apical area of 35 was adjacent to mental foramina and the cyst range was large, there could be issues of poor visual field, trauma, difficulty in apical preparation and backfilling after the apical resection. The satisfactory treatment effects might not be achieved, along with the risk of mental nerve injury, etc. The treatment suggestions were as follows: (1) the left mandibular second premolar 35 intentional plantations; (2) the left mandibular second premolar 35 was removed and implanted. The patient was introduced in detail to the methods, risks, and prognosis of the two treatments. The patient strongly desired to retain natural teeth and finally decided for the intentional replantation.
3. METHODS
The signed informed consent was obtained before the surgery. Before extracting the affected tooth, 9~10 mL of venous blood from the patient's forearm was taken in the centrifuge tube, which was used with the concentrated growth factor (CGF) centrifuge (Medifuge, Italy). The blood was centrifuged for 15 min according to the preset mode, where it was divided into 3 layers. The upper light-yellow layer (platelet-less layer) was discarded. The middle light-yellow translucent colloid layer (CGF layer) and the lower red colloid layer (red blood cell layer) were separated to prepare CGF for use.
The oral surgeon, under local anesthesia, performed minimally invasive tooth extraction by gripping the tooth with dental forceps and completely pulled out the left mandibular second premolar 35. The apical cyst and granulation tissue were removed with the hemostatic forceps to avoid contact with the instrument with the alveolar socket side wall. The alveolar socket was cleaned through repeated washings with sterile saline. The sterile wet gauze was placed at the extraction site for the firm patient bite. Endodontist treated the affected tooth, wrapped the isolated tooth in sterile gauze impregnated with normal saline, and examined under the microscope to confirm for no root cracks, perforations, and lateral root canals (Fig. 2A). Only the instrument separations were found at the apical hole (Fig. 2B). The isolated tooth was apicalized under a microscope, and root tip was removed by turbine emery needle of about 3 mm. The tip of the separating instrument was removed during rhizotomy, and the root canal was prepared by the ultrasonic tip of 3 mm in the reverse direction. Clean and dry nano-bioactive material (iRoot BP plus, Innovative Bio Ceramix Inc, Vancouver, BC, Canada) was used for the root tip backfilling (Fig. 2C), followed by polishing. Saline was injected during this process to moisten the isolated tooth. CGF was implanted into the alveolar fossa, and the isolated tooth was pressurized according to its dislocation direction. The replantation process was completed in 15 min. Periodontal fiber bands were used for the fixation, and occlusion was adjusted (Fig. 2D-E).
Postoperative management: antibiotics usage for 5 days (ornidazole 0.5 g, Bid, postprandial; Amoxicillin 0.5 g, Tid), gargle for 7 days with chlorhexidine gargle (10 mL, Tid) to prevent wound infection, suture removal after 7 days, and no bite of the hard object by the affected tooth in 3 months of surgery.
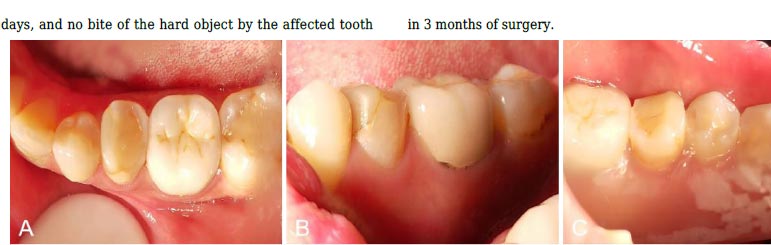
(A): 35 occlusal surface view; (B): 35 buccal view; and (C): 35 lingual view.
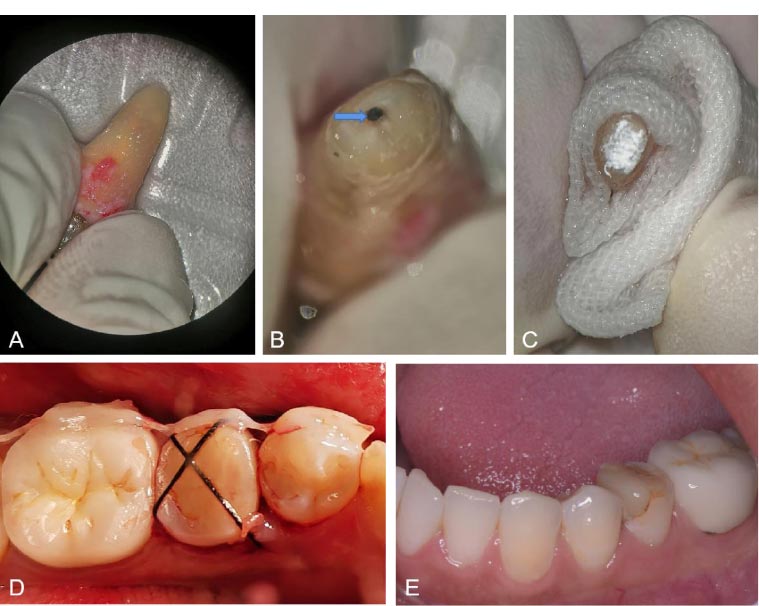
(A): Isolated tooth; (B): isolated tooth apex instrument separation; (C): iRoot BP root tip backfilling; (D): immediate replantation; and (E): 13 months of surgery.
4. RESULTS AND PROGNOSIS
The stitches were removed. The fixed fiber band was removed one week after the operation. The tooth extraction wound had mild edema, and the patient felt slight discomfort. Clinical examination: The degree of tooth looseness was I°. A reexamination was conducted 10 months after the surgery. The patient reported no spontaneous pain, no occlusal pain, and no gingival discharge. The clinical examination was normal, and the radiographs reflected that the apical area was reduced in projection and new bone was formed in the apical area (Fig. 3A-C). The clinical examination was normal, and no discomfort was found in the affected tooth at a follow-up of 13 months after the surgery (Fig. 3D, E). CBCT revealed that the new bone was further formed in the apical area, and bony plates were created in the bone destruction area. The density was close to that of the surrounding bone tissue (Fig. 3F, G).
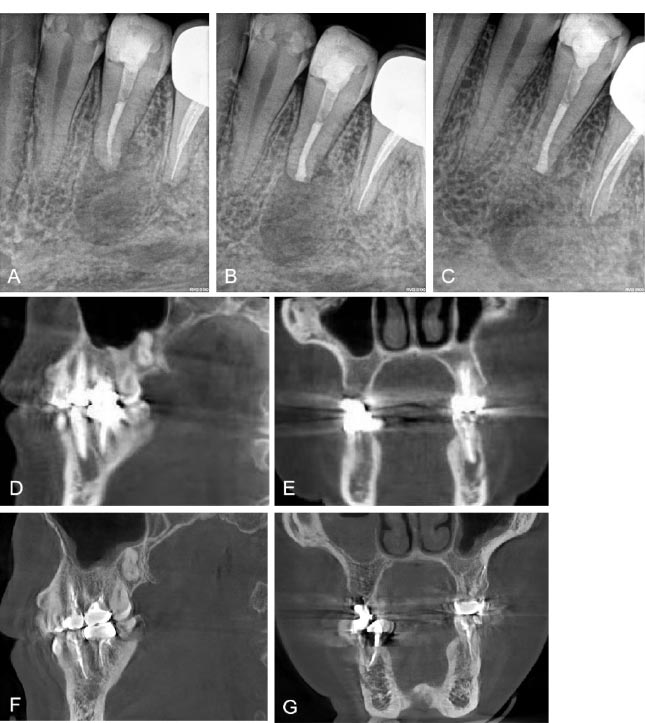
(A): Preoperative X-ray film; (B): immediate postoperative radiograph; (C): 10 months postoperative radiograph; (D): preoperative CBCT sagittal plane; (E): preoperative CBCT coronal plane; (F): 13 months postoperative CBCT sagittal plane; and (G): 13 months postoperative CBCT coronal plane.
5. DISCUSSION
Traumatic and avulsion tooth injuries are severe dental traumas that affect the pulp, periodontal membrane, alveolar bone, gum tissue, and other structures of the buccal cavity. When a tooth is dislocated from its socket, it disrupts the blood flow to the pulp and exposes periodontal membrane cells. The preferred treatment in these cases is tooth replantation. A successful re-attachment prolongs retention and improves aesthetics, occlusion, mastication function, and arch integrity. Intentional tooth replantation is often used as a last resort to preserve an undesired tooth [2], involving minimally invasive extraction, root evaluation, and lesion excision followed by replantation into the original socket [5].
Indications include non-treatable cases through non-surgical root canals, such as blockage in the root canal system or untreatable root canal wall perforation. Moreover, intentional replantation becomes vital in cases where apical surgery is not possible due to the limited surgical approach or visual field and proximity to the anatomical structures (e.g., mental foramen, mandibular neural tube, maxillary sinus, etc.). Furthermore, it is deemed fit where surgery might lead to periodontal tissue defects, and the refractory periapical inflammation is not favorable for traditional root canal therapy and surgery [6]. In this case report, the affected tooth 35 had undergone root canal treatment; however, the periapical tissue had inflammation, the apical tip was adjacent to the mental foramen, and 1/3 of the apical tip was relatively intact. The apical surgery herein could damage the mental nerve and destroy periodontal bone tissue. So, intentional replantation was tried to preserve the affected tooth. The cause of persistent inflammation could be identified and removed with direct vision from outside the body, especially when the lesion was placed in a location difficult to detect or impossible to operate in vivo, such as the instrument separation in 35 apical area of this case.
The intentional replantation success depended on the aseptic conditions of operation, the undamaged affected tooth extraction, periodontal membrane protection, in vitro operation time of the affected tooth, the bite force adjustment after replantation, and the postoperative compliance of the patient. Therefore, comprehensive clinical care of intentional replantation is crucial, which includes preoperative evaluation of the affected tooth; preparation and sterilization of the surgical area; preservation and restoration of the clinical crown; careful extraction and handling of the tooth; careful management of the alveolar socket and surrounding tissues; accurate alignment and stabilization of the external tooth root surface during replantation; precise placement and sealing of filling materials in the root canal system; proper reduction and retention techniques for optimal postoperative functional outcomes; and close monitoring for potential complications [7]. Tooth extraction was the most technical step in the process of intentional replantation [5]. The trauma to the tooth body and periodontal tissue was minimized during tooth extraction. In this case, the replanting process followed the principles of aseptic and minimally invasive surgery through conducive tooth extraction forceps. The forceps beak was located in the enamel cementum crown, and the affected tooth was dislocated from the alveolar fossa via the bucco-lingual shaking and slight twisting to avoid using dental supports for the smallest possible wound but maximum periodontal membrane preservation [7]. The in vitro operation time during intentional replantation had an effect on the maintenance of periodontal cell vitality. The in vitro operation time was shortened to minimize the damage and dehydration reaction of periodontal membrane cells. The replantation complications, such as alternative bone resorption and root resorption, could be avoided. In this case, the operation time was 15 min. The affected tooth was rinsed with normal saline to moisten the periodontal membrane, which improved its healing after affected tooth replantation. Kratchman [8] suggested keeping the in vitro time between 10 to 15 min, as the root resorption complications increased 1.7 times when time exceeded 15 min [9]. The periodontal membrane cell activity was essential for the tooth's survival after replantation. It was crucial to avoid excessive scratching of the tooth socket side wall and tooth root when removing the inflammatory tissue.
Moreover, the damage to residual periodontal tissue on the alveolar bone wall was avoided to promote the periodontal membrane healing after the surgery. In this case, a 3 mm root incision was performed to remove the instrument separation and infection lesion in the apical area of the affected tooth. The backward preparation and backfilling treatment were completed according to the standard. The iRoot BP plus to seal the root tip had good edge closure, biocompatibility, antibacterial property, and operability to provide responsive growth interface for periodontal membrane cells and osteoblasts, regeneration of periodontal membrane and bone tissue, and protection for later prognosis [10]. CGF was placed in the tooth alveolar socket before implantation. CGF was an anti-infection agent rich in growth factors that promoted multi-point osteogenesis and wound healing [11]. The reimplanted teeth loosening affected the periodontal tissue healing. The long-term loosening might form periodontal pockets, extend the epithelial attachment to the apical area, hinder the periodontal repair and bone regeneration, and adversely impact the prognosis [12]. Studies suggest that the affected tooth must be fixed with elastic splints for 7 to 10 days or 3 to 4 weeks after the surgery [2], however, the splints must not affect the oral self-cleaning.
In some cases, surgical sutures might be employed to cross the occlusal surface of the affected tooth [13]. Rouhani et al. proposed that the occlusion be adjusted after intentional replantation [4]. In this case, the periodontal fiber bands were utilized for the fixation and adjustment to avoid occlusal trauma, and to facilitate the alveolar bone reconstruction and periodontal membrane healing.
Extracadicular and alternative resorptions were the common complications of intentional replantation, with incidence from 0 to 35% [6]. Studies reported that the bone replacement resorption incidence in clinical practice ranged from 0 to 7%, while the exapical resorption ranged from 3.0% to 4.9% [14, 15]. However, the bone replacement root resorption process was slow in a non-inflammatory environment, and the affected tooth was maintained in the mouth for 5 to 20 years until the tooth root was absorbed and fell [16]. The affected tooth with bone replacement resorption remained in place and performed its function. Studies reported that bone resorption maintained the height and thickness of the alveolar ridge compared to the healing process of the alveolar socket after tooth extraction. The treatment complications of bone resorption could be regarded as another form of “site preservation”, which was conducive to the later dental implant or denture restoration [17]. Compared with the implant after extraction, intentional tooth replantation had the advantages of short operation time, less cost, less bone injury, and less limited by the anatomy and location.
Furthermore, the natural teeth had unmatchable advantages compared to the implant system. The natural teeth had proprioception and periodontal ligaments adapted to bite with force during chewing. Moreover, it was easier to maintain the gum anatomy for aesthetic effects [18].
CONCLUSION
In conclusion, clinicians should consider whether intentional replantation could be performed before dental implantation for the affected teeth with intractable periapical lesions. The affected tooth thus survived and was fully preserved with desired aesthetics, economy, and proprioception preservation. In clinical intentional replantation, the periodontal membrane should be protected, and in vitro operation time should be shortened with appropriate apical resection range and apical backfilling material. In this case, the patient underwent microscopic root canal therapy followed by intentional replantation and used nano-bioactive materials. The apical irritants were removed to control the infection at the core, preserve the affected tooth, and form new periodontal attachments. However, the efficacy needed further evaluations through long-term clinical follow-ups.
AUTHORS’ CONTRIBUTIONS
YA performed the surgery, QTY wrote the manuscript, YHW helped draft the manuscript, and SHL proofread the manuscript. All authors read and approved the final manuscript.
ETHICAL STATEMENT
Ethical approval was obtained from the ethics committee of the People’s Hospital of Xinjiang Uygur Autonomous Region (XJS20210119002).
CONSENT FOR PUBLICATION
Consent was obtained from the patient and parents of the patient for the publication of this report and any accompanying images.


