A Novel Design for Full-coverage Crown to Assist for Future Endodontic Treatment: A Survey on Difficulties of Access Cavity through Crowns and Pilot In-vitro Study Testing the New Design
Abstract
Aim
Many challenges are faced during opening cavity access through crowns. This study aimed to present a novel design for a full-coverage crown to overcome the difficulties of opening endodontic access and to facilitate root canal treatment.
Methodology
This study comprised two parts: (I) the survey, a cross-sectional questionnaire-based survey was conducted among dentists to assess the degree and type of challenges, complications and difficulties of opening the endodontic access cavity through zirconia and porcelain-fused-to-metal (PFM) crowns, and (II) the experiment, a novel crown design that include a mark occlusally as a guide to access precisely into the pulp chamber was fabricated by taking cone-beam computed tomography scans along with digital impressions of teeth prepared to receive zirconia crowns. The scans were merged with the digital impressions to detect the exact location of the pulp chamber and to make a guide on the crown over the pulp. Subsequently, the crowns were cut using a computer-aided design/computer-aided milling machine. Twenty-one samples in three equal groups (control 1, natural teeth; control 2, full zirconia crowns; and the experimental group, the novel design) were accessed by one operator. The following criteria were evaluated: time spent, quality, and size of the access cavity. The data were collected and analyzed using the SPSS software program at a significance level of P-value < 0.05.
Results
In total, 440 dentists from 28 countries participated in this survey. Generally, the participants reported moderate and difficult degrees of opening through crowns. The most reported challenges and complications were the time spent in the opening and the fracture or chipping of the crown material. For the experiment, no significant difference was found among the groups in relation to the time spent for opening (P = 0.57), with the least required time of access for the experimental group. In addition, no significant difference was found in the quality and size of the access cavity (P = 0.775) among the groups.
Conclusion
Endodontic cavity access through zirconia and PFM crowns is difficult and time-consuming. The novel proposed design utilizing digital dental technology can overcome these issues by preserving the crown, decreasing chair time, and providing less complicated treatment.
1. INTRODUCTION
Dental restorations with coronal coverage are highly predictable procedures to support and protect the remaining tooth structure after extensive loss [1], with a high survival rate (90.41%) up to 9 years [2]. Despite the predictable outcome, studies have reported a wide incidence rate of pulpal degeneration and/or disease, ranging from 2% to 33.8%, after placement of crowns in a period of up to 25 years [3-6]. Another study found that the survival rates for pulp vitality were approximately 84.4% for a single crowned tooth and 70.8% for a tooth used as an abutment after 10 years, which declined to 81.2% and 66.2% after 15 years, respectively [6]. Moreover, teeth with a history of multiple restorations have a higher risk of developing endodontic disease after crown cementation within 3 years than teeth without a history of multiple restorations [7]. Thus, clinicians and patients should be aware of possible future nonsurgical root canal treatment (NSRCT) whenever a prosthesis is placed.
The NSRCT of crowned teeth is a complicated procedure, practically and financially, where the crown is to be removed or accessed to enter the pulp chamber. Approximately 88% of endodontists, 69% of general practitioners (GPs), and 31% of prosthodontists obtain access to the pulp chamber through the crown and maintain the existing crown as the final restoration. Whereas only 7% of endodontists, 25% of GPs, and 34% of prosthodontists remove the crown, which involves a financial burden [8].
During the process of making a new crown or prosthesis, several factors affect its design, such as the position, inclination, and rotation of the teeth and the inclusion of several teeth in the prosthesis. In addition, intraoral periapical radiography may fail to show the location of the pulp chamber after prosthesis placement. Consequently, operators may face difficulties, and mishaps might occur while performing root canal treatment (RCT) through the crown because of the possible altered morphology [9]. Hence, dentists must use the best judgment and determine the trajectory to locate the pulp chamber, trying to avoid complications in the crown and/or tooth structure.
Upon literature search, no data are available on the types and levels of challenges and difficulties encountered during endodontic cavity access through full-coverage restorations. The aims of this study were twofold: (I) a survey was conducted to evaluate the degrees and types of challenges encountered in accessing the dental pulp through crowns, and (II) a novel design of full-coverage restoration with guided occlusal access to simplify and overcome the obstacles at the opening through the crowns was proposed.
2. MATERIALS AND METHODS
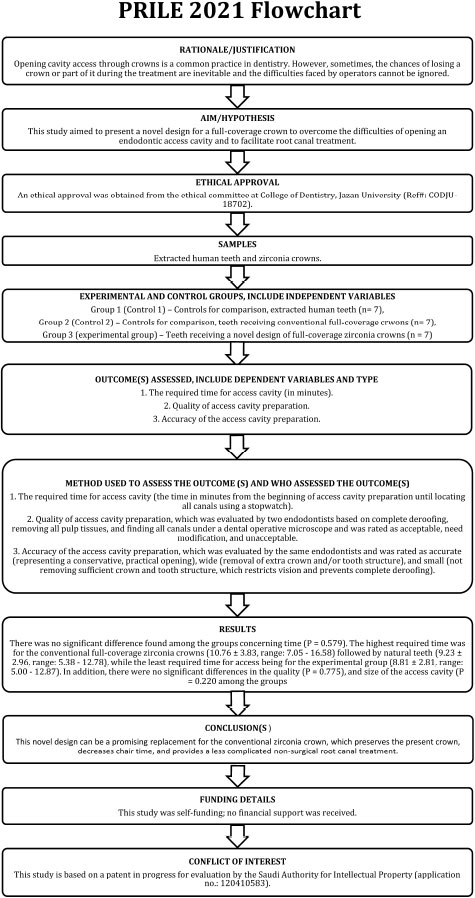
Before commencing the study, ethical approval was obtained from the ethical committee at the College of Dentistry, Jazan University (Ref#: CODJU-18702). The manuscript of this laboratory study has been written according to Preferred Reporting Items for Laboratory Studies in Endodontology (PRILE) 2021 guidelines [10, 11]. Fig. (1) shows the PRILE flowchart of the study. The PRILE checklist is found in the Table S1. The study comprised two parts.
| Question | Response | ||
|---|---|---|---|
| 1. What is your specialty? | Endodontist Non-endodontist | ||
| 2. What is your country of practice? | |||
| 3. How would you rate the difficulty of endodontic cavity access through PFM crowns based on your experience? | Easy | Moderate | Difficult |
| 4. What complications and difficulties did you encounter during endodontic cavity access preparation in full-coverage PFM crowns? | Multiple options | ||
| 5. How would you rate the difficulty of endodontic cavity access through zirconia crowns based on your experience? | Easy | Moderate | Difficult |
| 6. What complications and difficulties did you encounter during endodontic cavity access preparation in full-coverage zirconia crowns? | Multiple options | ||
2.1. Part I: The Survey
A cross-sectional survey was conducted globally to determine the degrees and types of difficulties and challenges encountered in opening endodontic cavity access through zirconia and porcelain-fused-to-metal (PFM) crowns. The questionnaire was designed and distributed electronically using Google Forms. The survey questions are shown in Table 1.
2.2. Part II: The Experiment
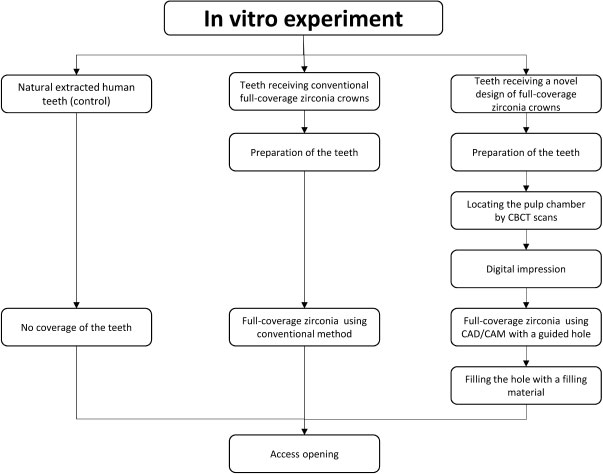
This pilot in vitro study included 21 extracted human mandibular first and second molars. Periapical radiographs were obtained for each tooth to evaluate its internal and external structures. Teeth with calcified pulp chambers and internal or external cracks were excluded. The teeth were fixed in resin blocks, kept in a wet environment (covered by wet gauze), and divided into three equal groups (N = 7) (Fig. 2):
Group 1 (control 1): Natural extracted human teeth,
Group 2 (control 2): Teeth receiving conventional full-coverage zirconia crowns, and
Group 3 (experimental): Teeth receiving a novel design of full-coverage zirconia crowns
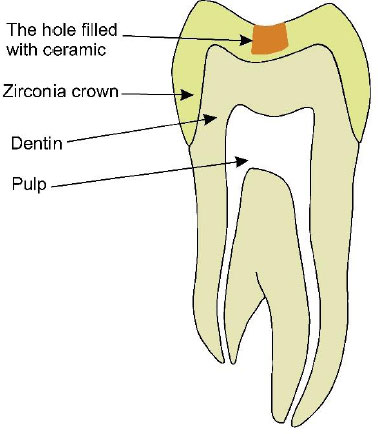
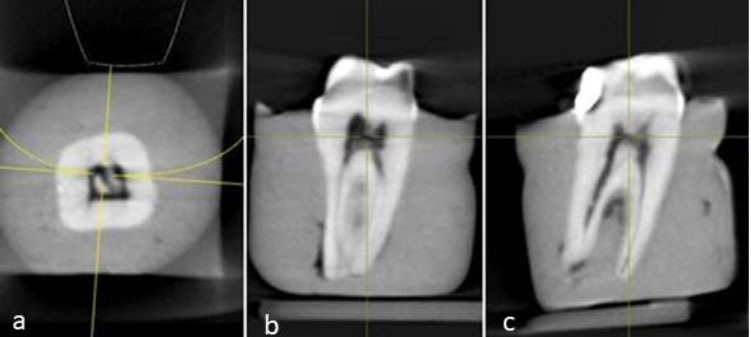
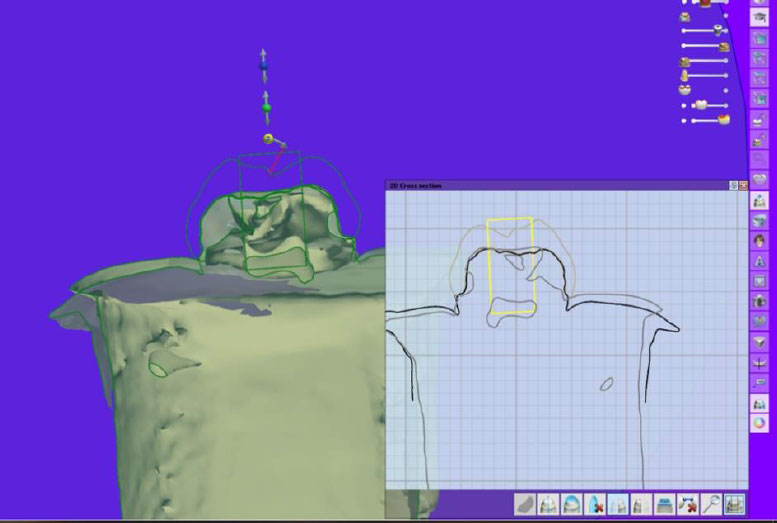
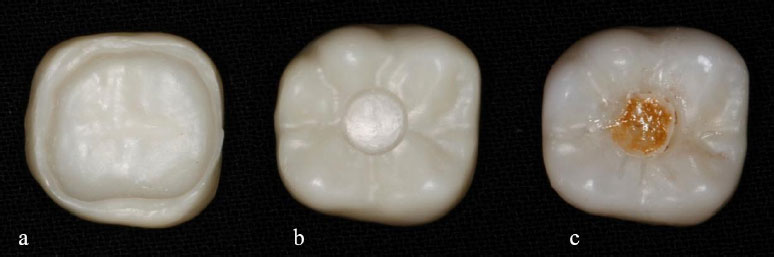
Teeth in groups 2 and 3 were prepared to receive full-coverage zirconia crowns using a course round-end taper diamond bur (BuraBraze Diamond, BR 6856.31.018, Brasseler, USA). A schematic representation of the novel design (group 3 experimental) is shown in Fig. (3). The novel design started by accurately locating the pulp chamber by taking cone-beam computed tomography (CBCT) scans (Sirona Galileos Compact, Germany) after crown preparation for each tooth (Fig. 4). Subsequently, the teeth were digitally scanned using an intraoral scanner (3Shape TRIOS, Denmark) to obtain a digital impression. The 3Shape software (3Shape Dental SystemTM, Denmark) was used to merge the CBCT and digital impression scans and locate the pulp chamber (Fig. 5). Full-coverage zirconia crowns (UPCERA ST, China) were then designed and cut using a computer-aided design/computer-aided machine (CAD/CAM) milling machine (Zirkonzahn, Italy) with a 3-mm-circle-radius hole over the detected pulp chamber. The hole was cut occlusal, leaving approximately 0.5 mm thickness as a base (Fig. 6a and b). The occlusal hole was filled with ceramic [VITA VM, VITA, Germany] of different shades as a guide for access through the crowns (Fig. 6c). Crown cementation for groups 2 and 3 was performed using dual-cure resin cement (RelyX UniCem, 3M, USA).
One operator performed the access cavity for all three groups using suitable coarse round and taper diamond burs (TIA DIAMOND, Tia Dent Inc., USA).. The following parameters were evaluated:
1. The required time for access cavity (the time in minutes from the beginning of access cavity preparation until locating all canals using a stopwatch).
2. Quality of access cavity preparation, which was evaluated by two endodontists based on complete deroofing, removing all pulp tissues, and finding all canals under a dental operative microscope, was rated as acceptable, needing modification, and unacceptable.
3. Accuracy of the access cavity preparation, which was evaluated by the same endodontists and was rated as accurate (representing a conservative, practical opening), wide (removal of extra crown and/or tooth structure), and small (not removing sufficient crown and tooth structure, which restricts vision and prevents complete deroofing).
The quality and accuracy were evaluated by Endodontists who evaluated and discussed together all samples and agreed on all findings. The data were collected, coded, double-checked and transferred to statistical software for analysis (SPSS v25, IBM Inc., Chicago, IL). The data were then subjected to normality tests, which revealed the non-normal distribution of the data (Shapiro Walk’s test; P< 0.05). The results were reported as frequencies and percentages (categorical variables) or mean and standard deviations (continuous variables). The Chi-squared test was used for the differences between groups in relation to the survey questions and the categorical variables in the experimental part, while the non-parametric Kruskal-Wallis test was used for the differences between the groups in relation to the continuous variables. A p-value < 0.05 was considered significant for all tests.
3. RESULTS
3.1. Part I: The Survey
In total, 440 dentists from 28 countries participated in this survey. Most participants were from Saudi Arabia (62.5%), India (7.5%), the USA (6.4%), and Egypt (5.7%). More than half of the participants were male (59.8%) and non-endodontists (55.7%). Table 1 shows the degree of difficulties reported by the participants for opening through the PFM and zirconia crowns. The overall self-reported degree of difficulties is shown in Fig. (7). Generally, the participants reported moderate and difficult degrees.
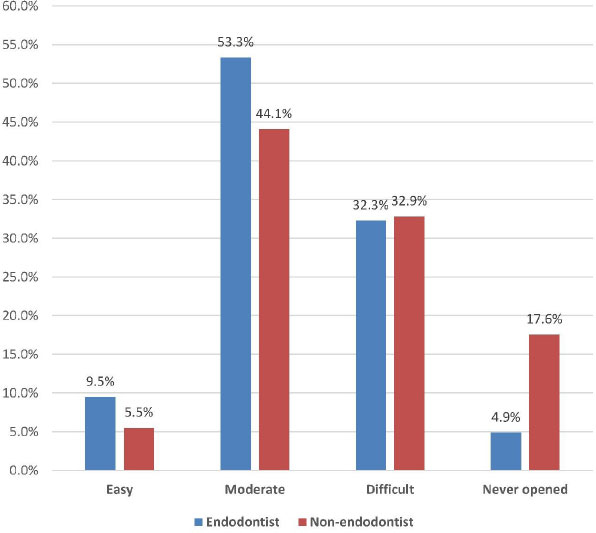
There was a significant difference (P < 0.001) between the endodontists and non-endodontists in the reported degree of difficulties of opening through the PFM crowns (χ2 = 33.728, P < 0.001). Approximately 56.4% and 28.7% of the endodontists reported moderate and difficult degrees, respectively. Whereas, 48.6% and 33.1% of the non-endodontists reported moderate and difficult degrees, respectively. Similarly, there was a significant difference between the endodontists and non-endodontists in the reported degree of difficulties in opening through the zirconia crowns (χ2 = 14.750, P = 0.002). However, the distribution of the responses was relatively different; 50.3% of the endodontists and 39.6% of the non-endodontists reported moderate difficulties, whereas 35.9% of the endodontists and 32.7% of the non-endodontists reported a difficult degree. Further details are presented in Table 2.
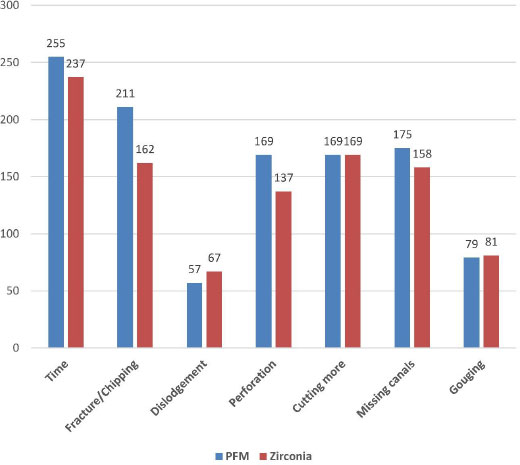
Regarding types of challenges, complications and difficulties, the most types reported by participants who opened through crowns (N = 402 for PFM crowns and N = 373 for zirconia crowns) were time spent in the opening and fracture or chipping of the crown material (particularly for PFM crowns). Further details are presented in Fig. (8).
| - | Easy | Moderate | Difficult | Never Opened |
|---|---|---|---|---|
| PFM crown | - | - | - | - |
| Endodontist | 26 (13.3) | 110 (56.4) | 56 (28.7) | 3 (1.5) |
| Non-endodontist | 10 (4.1) | 119 (48.6) | 81 (33.1) | 35 (14.3) |
| Total | 36 (8.2) | 229 (52.0) | 137 (31.1) | 38 (8.6) |
| Zirconia crown | ||||
| Endodontist | 11 (5.6) | 98 (50.3) | 70 (35.9) | 16 (8.2) |
| Non-endodontist | 17 (6.9) | 97 (39.6) | 80 (32.7) | 51 (20.8) |
| Total | 28 (6.4) | 195 (44.3) | 150 (34.1) | 67 (15.2) |
3.2. Part II: The Experiment
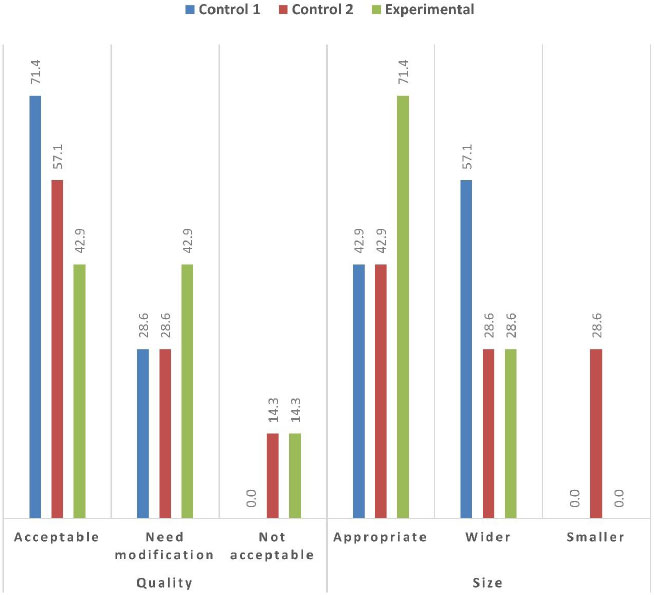
Table 3 shows the descriptive statistics of time among the different groups; no samples were lost during the experiment. There was no significant difference found among the groups concerning time (P = 0.579). The highest required time was for the conventional full-coverage zirconia crowns (10.76 ± 3.83, range: 7.05 - 16.58) followed by natural teeth (9.23 ± 2.96, range: 5.38 - 12.78), while the least required time for access being for the experimental group (8.81 ± 2.81, range: 5.00 - 12.87). In addition, there were no significant differences in the quality (P = 0.775) and size of the access cavity (P = 0.220) among the groups (Table 4 and Fig. 9).
| Group | Mean ± SD | Minimum | Maximum | P* |
|---|---|---|---|---|
| Non-crowned teeth | 9.23 ± 2.96 | 5.38 | 12.78 | 0.579 |
| Conventionally crowned teeth | 10.76 ± 3.83 | 7.05 | 16.58 | |
| Crowned teeth with novel design | 8.81 ± 2.81 | 5.00 | 12.87 |
| Group | Quality | - | Size | - | ||||
|---|---|---|---|---|---|---|---|---|
| Acceptable | Need Modification | Not Acceptable | P* | Appropriate | Wider | Smaller | P* | |
| Non-crowned teeth | 5 (71.4) | 2 (28.6) | 0 (0.0) | 0.775 | 3 (42.9) | 4 (57.1) | 0 (0.0) | 0.220 |
| Conventionally crowned teeth | 4 (57.1) | 2 (28.6) | 1 (14.3) | 3 (42.9) | 2 (28.6) | 2 (28.6) | ||
| Crowned teeth with novel design | 3 (42.9) | 3 (42.9) | 1 (14.3) | 5 (71.4) | 2 (28.6) | 0 (0.0) |
4. DISCUSSION
The primary objective of this study was to evaluate the feasibility of using a novel crown design for future endodontic treatment in terms of efficiency and practicality. Opening cavity access through crowns is a common practice in dentistry [8], with approximately 20%–50% of cases performed by endodontists through crowns [12]. After performing the root canal treatment through a crown successfully, the endodontic access will be restored with direct restoration [13]. Composite material is the common material as final filling of RCT to close the access cavity and ceramic crown repair. However, preparation for endodontic access at the occlusal surface of the zirconia crown can create microfractures and significant weakness of the crown leading to fracture of the crown [14]. In addition, zirconia material cannot be etched by acid and is complicated to achieve a high bonding surface [15]. Different surface treatments such as sandblasting, tribochemical silica, hydrofluoric acid or laser irradiation are proposed to improve the bonding [15]. Access through the crown and saving the tooth seem to be more appealing to patients than removing a crown; however, sometimes, the chances of losing a crown or part of it during the treatment are inevitable. In addition, the difficulties faced by operators cannot be ignored [9, 16].
Recently, multiple restorative materials have been developed for the fabrication of single-unit crowns. In our survey, we included only PFM and zirconia crowns because these two types are the most common materials used for posterior teeth owing to their high strength [17]. However, in the second part of this study (the novel design), the zirconia crown was selected because of its popularity, strength, wear compatibility with natural teeth, low cost, and high esthetics [17-20]. The fabrication of the specimens in zirconia with CAD/CAM technology aimed to unify the dimensions and shape of the specimens. In addition, the laboratory software allowed the merging of the digital impressions and CBCT scans to locate the pulp chamber of the virtual dice (of the scanned teeth) and accurately design the crowns for future endodontic access. This technology eases the repetition of our study worldwide and is not limited to zirconia material, but other materials can be used.
In the current study, 440 dentists from 28 countries reported moderate and difficult degrees of difficulty, with a significant difference between endodontists and non-endodontists. This is an expected result, which reflects the challenge faced by clinicians, where opening access through crowned teeth was reported by the American Association of Endodontics in endodontic case difficulty assessment forms and guidelines [9]. Consequently, time was the most common type of self-reported challenges . The difficulty of accessing through crowns and extended time of the procedure could be explained by the altered morphology of the crown and the self-non-guided trajectory by the operator, as he/she spends more time trying to open in the right spot over the pulp chamber. Endodontists have less difficulty opening through crowns, which is expected because more difficult cases are normally referred to them (had more experience).
Other reported complications with high prevalence included fractured or chipping parts, cutting more, perforations, missing canals, gouging and dislodgment of the crown. Lack of accuracy in locating the pulp chamber and canals can explain why clinicians cut more of the crown occlusal for visibility, which inevitably leads to the rest of the drawbacks and mishaps reported [21]. To fabricate the novel crown, CBCT was used to acquire the precise location of the pulp chamber after crown preparation to receive a zirconia crown. Regardless of CBCT's high cost, it has been widely used with a wide range of applications in dental practice, including endodontics, to appreciate root canal system variations and difficulties [22].
The least required time for access was observed in the experimental (novel design) group. This can be clearly explained by the presence of the guided access hole marked on the crown, which can save time in determining the appropriate access point. In addition, no significant difference was found in the quality and size of the access cavity among the groups, emphasizing the feasibility of the design and the possibility of its use for teeth with questionable RCT or susceptible endodontic retreatment. The thickness of zirconia at the base of the hall did not exceed 0.5 mm as the minimum required thickness that can withstand the physiological performance, regardless of the cementation type [23-25].
With the great advances in metallurgy of endodontic files that produced generations of efficient instruments [26]. These files help instrument root canals faster and more efficiently with resistance to cyclic fatigue and decrease canal transportation and lodging through small and conservative access cavities, which can work with our proposed design of precise guide to the pulp chamber of a given tooth without a need for extending the access cavity and jeopardize the strength of a crown or a tooth. In addition, the experiment was the initial prototype of our proposed idea and was not only limited to treated mandibular molar teeth with normal anatomy. The proposed idea can be conducted on any tooth type and in bridges or single crowns and even for teeth with previous root canal treatment or difficult internal anatomies, including extra canals [27].
This study has limitations. In the survey, the number of participants could be larger. However, the result seems significantly acceptable because the main reason for the survey was to establish real data about the difficulties of opening through crowns. Regarding the in vitro study, the number of samples was small; hence, the experiment could be considered a pilot and was conducted as the first prototype of a patent the main author was working on. The operator had never opened through a crown before and did not use any magnification aid during the experiment. This experiment could be improved by repeating the study with a larger sample size and more experienced operators to obtain more satisfactory outcomes. Another point not present in the experiment was the strength of the zirconia crown with guided access, which is considered in another experiment of this on-going project.
The future application of this technology is to simplify the access through the zirconia crown by modifying the material used in the guided opening area using different materials to ease access and maintain strength at the same time. In addition, it should be noted that this novel design is not specific to molar teeth. Still, the access hole can also be modified to fit the pulp chamber of other teeth type, including anterior, canine, and premolar teeth, following the pulp anatomy of each type. Moreover, the selection of a circle design, even though all teeth have known access cavity shapes [28], was because of the lack of designs in the 3Shape library. This could be another extension of the current project to include access cavity design for all teeth in the digital software library.
CONCLUSION
Considering the limitations of this study, accessing through crowns is an established difficulty that needs a real solution.
The proposed solution, with more studies and improvement, can be a promising simple replacement for the conventional or CAD-CAM crowns, which preserves the present crown, decreases chair time, and provides a less complicated NSRCT.
AUTHORS’ CONTRIBUTIONS
M.M. and H.A.A contributed to conceptualization, M.M., S.A.A., L.M.M., A.M.S., and A.M.J contributed to methodology, A.A. and S.B. contributed to software, and M.M. and A. A contributed to validation, M.Mcontributed to formal analysis, M.M. and A.R. contributed to data curation, M.M. contributed to writing—original draft preparation A.R. and M.A. contributed to writing—review and editing; M.M. supervised the study; M.M contributed to project administration. All authors have read and agreed to the published version of the manuscript.
LIST OF ABBREVIATIONS
| CAD/CAM | = Computer-Aided Design/Computer-Aided Machine |
| RCT | = Root Canal Treatment |
| NSRCT | = Nonsurgical Root Canal Treatment |
| GPs | = General Practitioners |
| PFM | = Porcelain-Fused-to-Metal |
| CBCT | = Cone-Beam Computed Tomography |
ETHICAL STATEMENT
Before commencing the study, ethical approval was obtained from the ethical committee at the College of Dentistry, Jazan University Ref.#: CODJU-18702.
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. The manuscript of this laboratory study has been written according to Preferred Reporting Items for Laboratory Studies in Endodontology (PRILE) 2021 guidelines.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors thank Mahmoud Rashid Al-Mahamid, Abdullah Mahnashy, and Sultal Jobahy for their valuable help in the lab.


