The Comparative Study on the Mental Index and Panoramic Mandibular Index in Thai Osteoporotic, Osteopenic, and Non-osteoporotic Patients: A Cross-sectional Study
Abstract
Background
Osteoporosis is one of the clinical problems in the elderly. Many previous studies focused on the index obtained from dental radiography as an adjunctive tool, which is considered beneficial for the screening of osteoporosis.
Objective
The purpose of this study was to compare the Mental Index (MI) and Panoramic Mandibular Index (PMI) acquired from panoramic radiographs in osteoporotic, osteopenic, and non-osteoporotic patients.
Methods
This research was approved by the Ethics Committee for Human Research, Srinakharinwirot University (certification number SWUEC-061/2562E). This study compared 150 osteoporotic patients undergoing treatment at the HRH Princess Maha Chakri Sirindhorn Medical Center with age-sex matched to 150 non-osteoporotic patients undergoing dental treatment at the Dental Hospital, Faculty of Dentistry, Srinakharinwirot University, using digital panoramic radiographs. MI and PMI were collected and analyzed using an independent T-test and Pearson correlation.
Results
The mean age of the 300 participants in the study was 57.82±12.25 years, while the mean age of the osteoporotic and non-osteoporotic patients was 57.95±12.30 years and 57.69±12.19 years, respectively. The mean MI for osteoporotic patients and non-osteoporotic patients was 0.314±0.088 cm and 0.3840±0.073 cm, respectively. Similarly, the mean PMI for osteoporotic patients and non-osteoporotic patients was 0.302±0.092 and 0.342±0.064, respectively. A significant difference in MI and PMI was observed between osteoporotic and non-osteoporotic patients (p=0.00).
1. INTRODUCTION
The advances in technology have led to longer life expectancy in people. Along with a decrease in the birth rate worldwide, the world is currently experiencing an inevitable aging of its population. Despite the statistics from past studies that showed an increase in the birth rate in African countries, the overall number of the world's aging people is still higher [1]. Thailand is one of many countries that is now undergoing a demographic transition towards an aging society. This change presents challenges for healthcare workers as there are numerous conditions associated with aging, such as dementia and osteoporosis.
Osteoporosis is a condition that affects the density of bones. It destroys bone structures on a microscopic level, making them weak and brittle and more prone to fractures [2]. It most commonly occurs in older people, particularly in postmenopausal women, due to a rapid decline in estrogen levels [3].
According to data from the Department of Medical Services, Ministry of Health, Thailand, osteoporosis is common in Thailand, particularly among women over the age of 50. It was found that 33% of women tended to develop the disease as compared to only 20% of men [2], corresponding with international studies revealing that in the United States of America, 50% of women and 20% of men over the age of 50 have osteoporosis. The Thai Osteoporosis Foundation (TOPF) declared that the number of patients with osteoporosis in Thailand is increasing every year; the number has increased by over 31% from 1997 to 2006. The number of patients with osteoporosis and aging people can be related, as the risk of developing osteoporosis increases with age [4].
Several techniques are available to measure bone density, with Dual-energy X-ray Absorptiometry (DXA) being the most commonly used method for diagnosing and monitoring osteoporosis due to its high accuracy and less invasiveness [5]. This method can also measure bone density at multiple sites at the same time, which is more convenient for diagnosis and analysis [6].
In addition to the aforementioned method, there have been studies aiming to use panoramic radiographs used in dentistry as a potential tool for examining and assessing the bone density of patients, including osteoporosis prediction. For example, in 2003, Lucchese and Manuelli explained bone biotypes in relation to the eruption of the third molar [7]. Currently, studies are being conducted on complementary methods used to help diagnose osteo- porosis using panoramic radiographs. It was found that variations in mandibular bone density are associated with changes in bone density in the alveolar bone and other bones. It was also found to be a more accurate predictor of osteoporosis than other bones in the body. As there is a higher rate of bone turnover than long bones, the alterations can be seen more clearly [8].
There are several radiographic indices used to assess the risk of osteoporosis, such as the Mental Index (MI), Mandibular Cortical Index (MCI), Gonial Index (GI), Antigonial Index (AI), and Panoramic Mandibular Index (PMI). These indices are based on landmarks under the mental foramen, an area used by many studies to assess them. This may be because fewer muscles are attached to this area. Even though there is a possibility of alveolar bone resorption, the distance between the mental foramen and the lower border of the mandible stays constant throughout one’s life [9, 10].
Mental Index (MI) is the most commonly used in studying osteoporosis as it is a reliable tool for diagnosing the disease in patients with lower bone mineral density [9] by measuring the width of the lower border cortex beneath the mental foramen. Panoramic Mandibular Index (PMI) is the ratio of the thickness of the mandibular cortex to the distance between the mental foramen and the lower border of the mandible. According to Benson et al. [10] and Ledger et al. [11], PMI has a higher efficiency in osteoporosis assessment than MI because PMI is a ratio value that accounts for panoramic radiograph distortion and magnification. Panoramic radiographs have been suggested as a tool for osteoporosis screening in both men and women. While osteoporosis is more prevalent in women, research has also focused on these radiographic indices in men. Dagistan and Bilge [12] investigated AI, MCI, MI, and PMI in 40 males, 20 of whom had osteoporosis, and the other 20 were healthy. They found that males with osteoporosis had significantly different AI, MI, and PMI compared to those without osteoporosis. These results were in agreement with the finding of a study by Bajoria et al., which reported that MI, MCI, GI, AI, and PMI could be effective screening tools for osteoporosis [13]. Additionally, Hastar et al. investigated MI, PMI, and MCI in 487 subjects aged 60-88 years with and without osteoporosis compared to dental conditions and sexes. Their study revealed statistically significant differences in MI and PMI between males and females, and all indices showed significant differences between subjects with and without osteoporosis. Those without teeth had lower MI and PMI indices compared to those with a partial or a complete set of teeth [14].
Güngör et al. [15] investigated the reliability of the PMI in assessing individuals with osteoporosis. The study concluded that the reliability of PMI relies on the ability to precisely determine the extent of the mental foramen. Similarly, Govindraju and Chandra [16] studied MI and PMI in both males and females. Their findings further highlighted the importance of excluding people from the study group when the location and extent of the mental foramen cannot be clearly identified on the panoramic radiograph. The study found significant statistical differences between males and females for both MI and PMI.
Currently, there is limited research available regarding the relationship between MI, PMI, and osteoporosis in Thailand. Rangsiyanon et al. [17] conducted a study on the use of MI and PMI for clinical osteoporosis assessment in Thailand. The study revealed a significant difference in MI and PMI between the Thai population aged 20-30 years (with high bone mass) and individuals over 60 years of age (with lower bone mass than younger individuals) when age was used as a criterion for classification. However, when gender was used as a criterion, only MI showed significant differences. These findings indicated that MI and PMI can aid in an assessment or screening for initial osteoporosis risk. Therefore, if dentists can use panoramic radiographs in the preliminary assessment of osteoporosis from the mandible bone, patients may receive a diagnosis from physicians in the early stages of the disease and even increase success in preventing or alleviating osteoporosis as well.
The purpose of this study was to compare MI and PMI acquired from panoramic radiographs in osteoporotic, osteopenic, and non-osteoporotic patients.
2. MATERIALS AND METHODS
This research was approved by the Ethics Committee for Human Research, Srinakharinwirot University, certification number SWUEC-061/2562E.
2.1. Sample Selection
The sample selection criteria for the present research study were as follows:
2.1.1. Inclusion Criteria
Female patients who have had an osteopenia or osteoporosis diagnosis at the Osteoporotic clinic of the HRH Princess Maha Chakri Sirindhorn Medical Center, Faculty of Medicine, Srinakharinwirot University, were diagnosed with osteoporosis if their DXA score was less than -2.5, and with a DXA result between 0 and -2.5 and were diagnosed with osteopenia, were included in this study.
The control group consisted of individuals who self-reported that they do not have osteoporosis and underwent dental treatment at the Dental Hospital, Faculty of Dentistry, Srinakharinwirot University, and whose age and sex matched the experimental group.
These selection criteria were carefully designed to ensure a representative sample of the patient population and to maximize the validity of the study's findings.
2.1.2. Exclusion criteria
An important factor that would exclude patients from the study was the patient's medical history, particularly their prior usage of medications purportedly linked to both metabolism and a reduction in bone mass density [18], which can be classified as follows:
- Patients with a history of hyperparathyroidism, hypoparathyroidism, diabetes, kidney failure, hypogonadism, pituitary adenoma, Addison’s disease, Cushing’s disease, liver failure, Ankylosing spondylitis, rheumatoid arthritis, malnutrition, multiple myeloma, and anemia.
- The use of the following drugs that affect bone metabolism: corticosteroids, anticoagulants, chemotherapy, epilepsy drugs, thyroid hormone drugs, diabetes drugs, antihypertensive drugs, and lipid-lowering drugs.
- Patients with a history of bone fractures, radiotherapy, bone graft or bone destruction in the study area.
- Patients who regularly smoke and/or consume alcoholic beverages, as these behaviors can reduce the efficiency of calcium absorption in the body.
- Patients who have been formerly diagnosed with osteoporosis and/or using medications to treat osteoporosis bone, such as calcitonin, bisphosphonates, fluoride, hormone replacement therapy, calcium, and vitamin D.
2.2. Data Collection
Data was collected by three investigators, with inter-examiner calibration using the number of the population representing 5% of the total population. The Kappa coefficient for measuring MI and PMI were 0.71 and 0.84, respectively.
The radiographs obtained were interpreted with a Picture Archiving and Communication System (PACS) reader on the same computer and monitor at the Oral Medicine and Oral Disease Diagnosis Clinic at Dental Hospital, Faculty of Dentistry, Srinakharinwirot University. The two targeted indices were measured according to the following procedure:
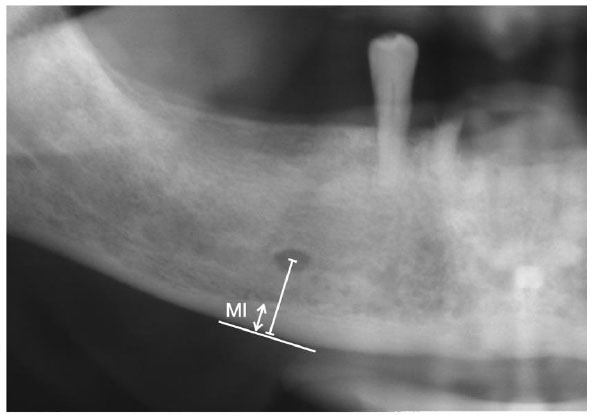
1. MI can be measured by drawing a line perpendicular to the lower border cortex of the mandible through the center of the mental foramen. Then, along this line, the width of the mandibular cortex is measured (Fig. 1).
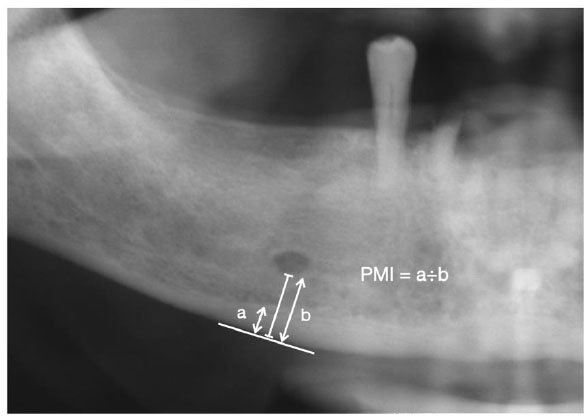
2. PMI can be measured by drawing a line from the lower border of the mental foramen perpendicular to the lower border of the mandible and then finding the ratio between the thickness of the mandibular cortex and its length from the lower border of the mental foramen perpendicular to the line of contact with the lower border of the mandible (Fig. 2).
2.3. Statistical Analysis
The data obtained in the study were analyzed and interpreted utilizing SPSS version 23.0 (SPSS Inc., Illinois, USA). The normal distribution within the population was verified via the Kolmogorov-Smirnov test. Upon confirmation of normal distribution, an independent sample T-test was conducted. Conversely, if the data sets were considered non-normally distributed, the Mann-Whitney U test was performed. The confidence coefficient was set at 0.95 to study the contrast of the two indices. Subsequently, a Pearson product-moment correlation analysis was carried out to examine the correlation and trend between the two indices.
3. RESULTS
The present study involved data collection from 150 osteoporotic patients at the Clinic of Osteoporosis, HRH Princess Maha Chakri Sirindhorn Medical Center, Faculty of Medicine, Srinakharinwirot University. These patients were age-sex matched with a control group of 150 dental patients from the Dental Hospital, Faculty of Dentistry, Srinakharinwirot University, who reported no osteoporosis history. Panoramic images were then analyzed using NNT viewer and SoliPACS program. Age, MI, and PMI were used for statistical analysis. Results indicated that the osteoporotic patients had an average age of 57.95±12.30 years, whereas the average age of healthy patients was 57.69±12.19 years. The findings revealed no statistically significant difference in age between the two groups (P = 0.881). Of the 150 patients in the study group, 82 (54.67%) were diagnosed with osteoporosis, while 68 (45.33%) were diagnosed with osteopenia.
The examination of MI revealed that patients with osteoporosis exhibited an MI of 0.314±0.088 cm, while the control group demonstrated an MI of 0.384±0.073 cm. The results indicated a statistically significant difference in MI between the two groups (P = 0.00). Similarly, the patients with osteoporosis and the control group displayed a PMI of 0.302±0.092 and 0.342±0.064, respectively. The findings revealed that patients with osteoporosis had a significantly lower PMI than the control group (P = 0.00) (Table 1).
Table 1.
| - | Osteoporotic Group (mean ± SD) |
Control Group (mean ± SD) |
P-value |
|---|---|---|---|
| Age (years) | 57.95±12.30 | 57.69±12.19 | 0.881 |
| MI (cm.) | 0.314±0.088 | 0.384±0.073 | 0.000* |
| PMI | 0.302±0.092 | 0.342±0.064 | 0.000* |
The statistical analysis demonstrated a correlation coefficient of 0.636 between the two indices, indicating a strong positive relationship between them with an agreement rate of 99%.
4. DISCUSSION
Numerous studies have investigated the potential of panoramic radiographic indices for screening and diagnosis of osteoporosis. Such imaging techniques are readily accessible in dental settings and can offer an efficient and cost-effective approach to identifying patients with osteoporosis. In 2017, Rungsiyanont et al. [17] explored MI and PMI in four distinct groups: young males, older males, young females, and older females. The results revealed significant differences in MI among young males and females, while PMI showed significant differences between young males and females and older females. Later, in 2018, Rungsiyanont et al. [19] conducted a more focused investigation by segmenting the population into 3 groups: young males, young females, and older females. According to our findings, there were statistically significant differences in MI and PMI between all 3 groups. The findings in our study suggest that age and sex play a role in influencing MI and PMI. Only 2 categories of older patients, namely males and females, were investigated by Talungchit et al. with respect to MI and PMI. Statistics revealed that there was no statistically significant difference in the MI. However, there was a statistically significant difference in the PMI [20]. The inclusion criteria of this present study were based on the previous studies, focusing on female patients who have osteoporosis and osteopenia.
Most prior studies were focused on the relationship between age, sex, and osteoporosis. However, in this present study, researchers focused on examining the differences between MI and PMI in patients with and without osteoporosis to examine how osteoporosis affects MI and PMI. The study group in this research were 150 patients who had been diagnosed with osteopenia or osteoporosis at the Osteoporotic Clinic of the HRH Princess Maha Chakri Sirindhorn Medical Center, Faculty of Medicine, Srinakharinwirot University and 150 individuals without osteoporosis, who underwent dental treatment at the Dental Hospital, Faculty of Dentistry, Srinakharinwirot University, and whose age and sex matched the experimental group. According to the findings of this study, osteoporosis had a statistically significant impact on MI, which is consistent with the findings of a study by Marandi et al. [21]. The panoramic radiographs of 67 females aged between 36-92 years were studied, and it was found that MI in osteoporosis patients was significantly different in comparison to those of healthy individuals. In the present study, the mean MI of patients without osteoporosis was higher than patients with osteoporosis, i.e., 0.384±0.073 cm and 0.314±0.088 cm, respectively. The results were consistent with previous studies by Akshita and Asha [22] and Kribbs [23] that reported that females with no osteoporosis had a higher MI than females with osteoporosis. Dargiston and Bilge [12] also conducted a study, in which they compared the MI of 20 osteoporotic males and 20 males without osteoporosis. The results from both groups were statistically different. Specifically, MI in osteoporotic males was significantly lower than that of males without osteoporosis. Mansour et al. [24] had the same design as employed in this present study, which focused on indices from panoramic radiographs in predicting osteoporosis and found a positive correlation between MI and PMI. This study, however, contrasted the findings of a study by Pornsathapan [25], who reported that the MI determined from panoramic radiographs in patients with hip bone fractures was not statistically significantly correlated with the patients’ bone density.
Regarding PMI, the present study found that the mean PMI in patients with and without osteoporosis were 0.302±0.092 and 0.342±0.064, respectively. The mean PMI in patients with osteoporosis was statistically significantly lower than in patients without osteoporosis. This finding was found to be consistent with a study by Akshita and Asha [22], stating that females without osteoporosis had a higher PMI than those with the disease. Furthermore, Dargiston and Bilge [12] concluded in their study that PMI measured from males with osteoporosis was statistically significantly lower than PMI measured from males without osteoporosis. Moreover, Horner and Devlin [26] investigated PMI in females with and without osteoporosis. The results revealed that PMI values in both groups were significantly different. Therefore, it is possible to conclude that PMI can be used for the diagnosis of mandibular osteoporosis.
The PMI results obtained in this study contradict the findings of a study by Marandi et al. [21], who discovered that the PMI of those with normal bone mass and patients with osteoporosis were not statistically different. Pornsathapan [25] also reported that PMI received from panoramic radiographs of patients with hip bone fractures did not statistically significantly correlate with the patients’ bone density.
Based on the statistical analysis of the correlation between MI and PMI, it was found that the correlation was 0.636, which was positive, and a high correlation at 99%. These findings were consistent with those reported in a study by Bajoria et al. [13], who reported a positive correlation of 69.57% and a high correlation. Therefore, our results suggested that there was a significant relationship between MI and PMI, as demonstrated by the high correlation coefficient. However, further studies are also required, in which DXA, MI, and PMI indexes in osteoporotic, osteopenic, and healthy patients should be monitored and obtained on the same day. The correlation of these indices may be more conclusive and affirmative for clinical applications of these indices.
CONCLUSION
Based on the analysis of two populations, this study demonstrated statistically significant differences in MI and PMI between the two groups. Specifically, the group with osteoporosis exhibited lower values of both indices compared to the non-osteoporotic group. However, it is worth noting that some osteoporotic individuals had equal or higher values of these indices than the non-osteoporotic group. This unexpected finding could be from various factors, such as misdiagnosis, medication regimens or the period of treatment of this group. Concisely, medical factors, such as the type, method, and duration of drug administration, may impact these index values. Therefore, these findings raise interesting questions to be focused on in further investigations in the future.
AUTHORS’ CONTRIBUTIONS
ST and SR contributed to the conception, design, data analyses, and interpretation of the study. ST, KT, and SR participated in the provision of study materials and/or patients, data collection, and assembly.
LIST OF ABBREVIATIONS
| MI | = Mental Index |
| PMI | = Panoramic Mandibular Index |
| MCI | = Mandibular Cortical Index |
| GI | = Gonial Index |
| AI | = Antigonial Index |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was approved by the Ethics Committee for Human Research, Srinakharinwirot University, certification number SWUEC-061/2562E.
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2015.
AVAILABILITY OF DATA AND MATERIALS
The datasets used during the current study can be made available upon reasonable request to the corresponding author [S.R.].


